Preventing Infectious Diseases: OSHA’s Stance on Bloodborne Pathogens
Generally, professionals in healthcare settings are well-acquainted with the significant threat of infectious diseases via bloodborne pathogens. However, their potential health hazards extend beyond the scope of the healthcare industry. On that account, understanding the fundamentals of bloodborne pathogens and the associated risks is essential for all.
Therefore, within the parameters of this blog, we will explore bloodborne pathogens, their mode of transmission, the potential risks they pose to the workforce, and the key takeaways you can enforce to protect yourself and others around you.
What are Bloodborne Pathogens?
Simply put, bloodborne pathogens, commonly found in human blood and certain bodily fluids, are infectious microorganisms transmitted via direct contact with infected blood or potentially infectious materials, posing a severe threat to individuals who come into contact with them.
Most Common Bloodborne Pathogens:
Bloodborne Pathogens, primarily viruses and bacteria, are most commonly prevalent in the blood and can give rise to various infectious diseases when transmitted to others. The most common bloodborne pathogens include:
- Hepatitis B Virus (HBV): A highly contagious viral infection lasting up to seven days outside the body, HBV generally affects the liver, leading to acute and chronic hepatitis. Its symptoms can range from mild illness to fatally damaging the liver.
- Hepatitis C Virus (HCV): primarily affecting the liver; HCV is a chronic infection that can lead to severe liver damage over a specific period. Though it doesn’t have a proper vaccine like HBV, it can be cured with appropriate antiviral medications.
- Human Immunodeficiency Virus (HIV): HIV is a deadly virus that targets the human body’s immune system, weakening its ability to fight infectious diseases. When left untreated, HIV can become an acquired immunodeficiency syndrome (AIDS), a severe form of HIV infection.
- Human T-Cell Lymphotropic Virus (HTLV): HTLV is a group of viruses that can lead to various diseases. HTLV-1, in particular, is associated with adult T-cell leukemia and a neurological disorder called HTLV-1-associated myelopathy/tropical spastic paraparesis (HAM/TSP).
Statistics About Bloodborne Pathogens
To understand the risk associated with bloodborne pathogens, it’s important to look at the numbers.
- The CDC estimates that 5.6 million workers in the healthcare industry and related occupations are at risk of exposure to bloodborne pathogens. (OSHA)
- The CDC reported 57 documented cases and 140 possible cases of HIV transmission to U.S. healthcare workers between 1981 and 2006. (CDC)
- Approximately one in five (18.9%) tattooists in a study reported having needlestick injuries and lacerations while undergoing their work. (NCBI)
How Can Bloodborne Pathogens be Transmitted in the Workplace?
The most common transmission routes through which bloodborne pathogens are generally transmitted are:
- Needlestick Injuries: Accidental cuts or punctures with contaminated sharp objects such as needles can expose individuals to infectious diseases.
- Contact with Contaminated Surfaces: Individuals in workplaces where proper hygiene and disinfection practices are not enforced may encounter surfaces, devices, or equipment contaminated with blood or bodily fluids.
- Mucous Membrane Contact: Bloodborne pathogens can enter the body via mucous membranes in the eyes, nose, and mouth.
- Open Skin Lesions or Cuts: Bloodborne pathogens can enter the bloodstream through open wounds, cuts, or skin lesions that come into direct contact with infected blood or fluids.
Factors Increasing the Risks of Transmission:
- Lack of Vaccination: Workers unaware of their infection status or those not vaccinated pertinent to the infectious disease are more likely to infect others.
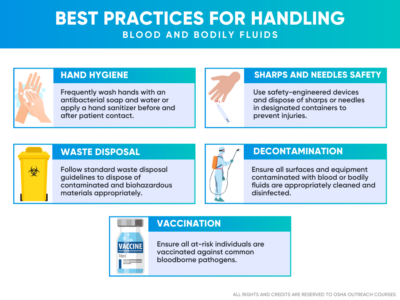
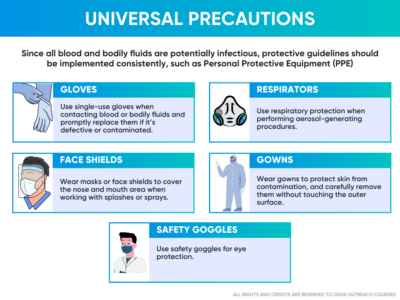
- Poor Infection Control Practices: Inadequate access and use of Personal Protective Equipment (PPE) such as safety gloves, gowns, masks, and eyewear, as well as improper handling and disposal of contaminated/hazardous materials, can cause exposure to bloodborne pathogens.
- High-Risk Occupations: Occupations including but not limited to healthcare, emergency response, and law enforcement carry a high risk of exposure to bloodborne pathogens due to the nature of the work.
- Failure to Follow Universal Precautions: When left untreated, infectious blood and bodily fluids often result in unsafe practices and increase the likelihood of spreading infectious diseases.
Are You at Risk of Exposure to Bloodborne Pathogens?
Following are the individuals who are at the potential risk of acquiring exposure to bloodborne pathogens:
- Hazardous Waste Handling: Individuals in workplaces where hazardous waste is frequently generated, including manufacturing, healthcare, construction, and research facilities, may come into contact with contaminated materials, which are the primary source of bloodborne pathogens.
- First Aid and Emergency Response: First responders, including police officers and firefighters, who provide first aid or respond to workplace incidents may encounter situations involving blood or bodily fluids. In addition, paramedics and emergency medical technicians (EMTs) may face circumstances requiring them to dispense care to individuals with unknown infection statuses, elevating their risk of exposure.
- Maintenance and Custodial Staff: Workers tasked with cleaning and maintaining industrial facilities may come across contaminated materials when treating medical waste containers, cleaning up after injuries and accidents, or disposing of used medical supplies.
- Construction Industry: Employees in the construction sector have a higher chance of getting exposed to bloodborne pathogens, specifically when they encounter hazardous materials, biohazard spills, or unpredictable accidents on job sites.
- Laboratory Personnel: Laboratory Personnel, including technicians and researchers, are primarily at the potential risk of exposure to bloodborne pathogens when handling, collecting, processing, and assessing blood and bodily fluids specimens or spills if appropriate safety precautions are not followed.
How Can Workplaces Comply with OSHA Regulations to Reduce the Exposure to Bloodborne Pathogens?
The primary goal of OSHA is to ensure workplace safety in all spheres of occupations. Therefore, the OSHA online training covers all fundamental safety topics, including bloodborne pathogens, to ensure the well-being of workers, specifically in workplaces where they may face exposure to blood and other potentially infectious materials (OPIM).
Since OSHA’s Bloodborne Pathogens Standard (29 CFR 1910.1030) mandates safety training requirements, it is advised for all to enroll in the OSHA 30-Hour Construction Training Course and OSHA 30-Hour General Industry Training Course to ensure that all at-risk employees acquire sufficient knowledge on bloodborne pathogens to identify, control and mitigate exposure. In addition, you can also enroll in the Bloodborne Pathogen Certification course, specifically designed to dispense knowledge on Bloodborne Pathogens. Hence, all workplaces will be able to meet compliance with OSHA regulations.
Upon completing OSHA safety training, workers will become aware of the following objectives to enforce and promote workplace safety:
- Develop an Exposure Control Plan: Draft a detailed control plan that mainly outlines the essential safety measures such as emergency response, engineering controls, work practice controls, and the use of PPE. The risks of exposure will be reduced since failing to do so can result in hefty penalties from OSHA inspections.
- Early Detection and Immunization: Stay updated with vaccinations for timely medical treatment to prevent disease progression.
- Occupational Safety: Employers will ensure that the workforce has proper access to occupational health services for medical evaluation, counseling, and follow-up upon exposure to accidents.
- Use Self-Assessment Checklists: Individuals will compare their knowledge and expertise to the self-assessment checklists. Self-assessment checklists include information on transmission routes, use of PPE, and emergency response to exposure accidents.
- Stay Updated: Research on bloodborne pathogens to stay updated on the latest OSHA regulations and best practices to ensure safety.
- Foster a Safe Workplace Culture: Encourage open communication among employees regarding safety concerns and the immediate reporting of exposure incidents. Employers recognizing and rewarding such behaviors will further boost employees’ morale to make the organization a better workplace for all.
- Regular Inspections: Perform regular audits and inspections to examine and evaluate OSHA compliance with safety practices and determine improvement areas.
Conclusion
Preventing bloodborne pathogens from infecting workers is the responsibility that lies with employers, unions, employees, and government institutions alike. OSHA has set standards regarding these hazards that workplaces must enforce to avoid the spread of diseases and keep their workers safe from the long-term effects of exposure.